The intrauterine device (IUD) and the intrauterine system (IUS) have a long and complicated history. The IUD is a contraceptive device inserted into the uterus, which serves as a physical barrier to prevent sperm from fertilizing the egg. Its earliest form can be linked to the work of Ernst Gräfenberg[1], who in 1929 created the ring IUD (Thiery 1997). Over the course of several decades, the IUD was constructed and re-constructed in terms of the materials used, its physical shape, and its promotion to women. Through the development process, some devices, such as the Dalkon Shield, caused irreparable damage. In 1969, the first copper IUD was created by Jaime Zipper and Howard J. Tatum, which took the now easily recognizable T-shape form. While the copper IUD was considered successful in terms of its ability to prevent pregnancy, women commonly had it removed due to increased bleeding during menstruation. Subsequently, the intrauterine system (IUS) was created, first by Antonio Scommegna in the 1960s using progesterone and later by Tapani Luukkainen in 1976 using levonorgestrel; this shift increased its effectiveness from a duration of one year to five years. After over a decade of testing, the Mirena IUS was released in Finland – it would not be approved for sale in the United States until 2001.
As of 2019, the IUD accounts for 7.9% of contraceptive use in Europe and North America, which has nearly doubled since 2011. In recent years, insertion rates and concern regarding sexual and reproductive rights have increased both in the United States and Canada with the election of conservative politicians. While conducting ethnographic fieldwork from within a sexual health centre and aboard a mobile sexual health clinic in Toronto, I saw first-hand the rising popularity of the IUD/IUS. The Centre set a daily limit for insertions, ranging from one to four slots per day. Such limitations were necessary to accommodate the increased time spent counseling, completing the procedure, and potentially dealing with complications. I would arrive for my volunteer shift and see women lined up against a wall, some sitting and listening to music while others stood and looked at their phones. Many were waiting for the clinic to open in hopes of receiving one of these coveted spots for IUD/IUS insertion.
In recent years, anthropologists, STS scholars, and feminists have sought to unpack what technology means, what it signifies, and how we understand it in context (see Manderson 2012; Davis 2015). Technologies are never just material objects – they are created and have the power to create. Furthermore, they are not neutral. In this post, I argue this is a productive framework to understand the intrauterine device and the intrauterine system. The creation, circulation, and promotion of these sexual health technologies are directly tied to political, moral, and neoliberal discourses. For example, the IUD was constructed as a technology of population control in the Global South via family planning projects while being marketed as a technology of empowerment and as a lifestyle contraceptive in the United States for white middle-class women (see Takeshita 2012). The IUD/IUS holds multiple moral investments, and while it is popularly understood and promoted in terms of sexual and reproductive choice, this does not mean it operates outside of such histories. I offer the following two ethnographic vignettes to illustrate how the IUD/IUS as a sexual health technology is constructed via discourses and practices of empowerment and governance.
Pharmaceutical Representatives in the Clinic
An IUS model given to staff and volunteers at The Centre for promotional purposes. Photo by the author.
Upon arriving at The Centre, a moderately-sized sexual health clinic in downtown Toronto, I grab some scrap paper and a pen before heading into the makeshift conference room (a space where staff and volunteers normally eat their lunch). There is a man speaking with a few of the counselors, holding a black briefcase. I do not learn the purpose of his visit until the monthly staff meeting begins. Katherine[2], the administrative coordinator, hands out sample intrauterine systems (IUS) – they are wrapped in plastic with a tiny tag that reads “Kyleena.”
We are told the Kyleena, commercialized by the pharmaceutical company Bayer, is another option for clients wishing to have an IUS inserted. Using the information provided by the sales representative, Katherine explains how Kyleena is slightly smaller than another popular IUS (the Mirena) and offers an option for users who would like a device with fewer hormones – Mirena contains a total of 52mgs while Kyleena has only19.5mgs. We are also told there is a website that can help those seeking contraception to decide on the right method.
The Mobile Clinic and Contraception
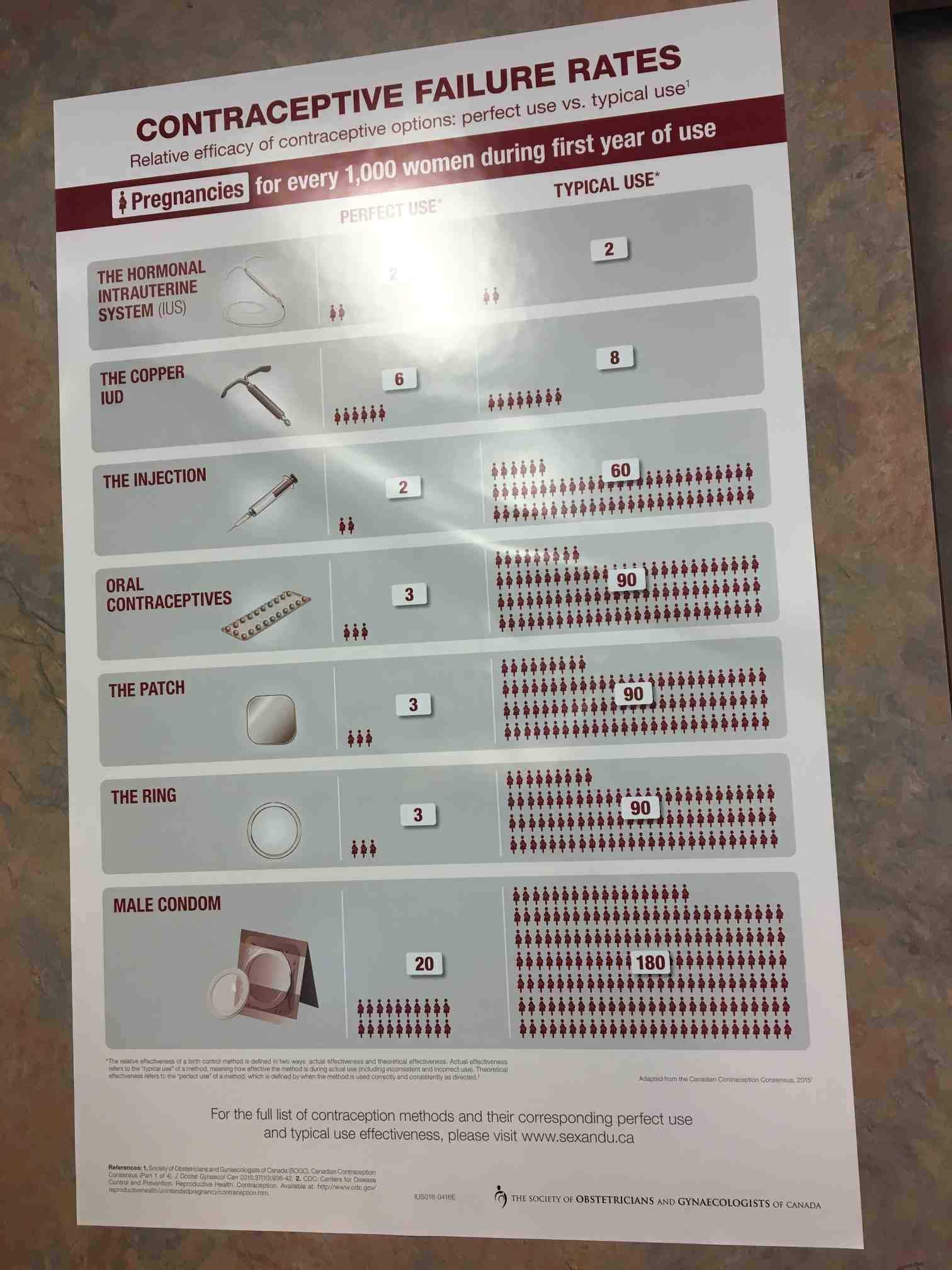
A poster, created by The Society of Obstetricians and Gynecologists of Canada, affixed to one of the walls of the mobile clinic. Photo by the author.
Contraceptive choice is a topic frequently woven into conversations aboard The Mobile, a retrofitted Winnebago used to deliver sexual health care services across the Greater-Toronto-Area. This clinic is used to deliver care primarily to marginalized, racialized, and immigrant communities. During a brief period of downtime, after all clients who have come aboard the bus have been seen by Aaliyah (the counselor) and Dr. Shereen (the attending physician), we begin to talk about a poster tacked to the wall above the printer.
The poster outlines multiple forms of contraception, from male condoms to the IUS, and it is apparent to the three of us that it was created to convey the most effective – and foolproof – ways to prevent pregnancy. As I take a photo of the poster, both women offer insight into this hierarchy of contraception by drawing on their experiences working in sexual health care. According to Dr. Shereen, doctors are encouraged via financial incentives to prescribe intrauterine systems such as the Mirena. Aaliyah describes the ways in which the IUS is not always provided with informed consent, as one of her clients, a young woman of color, did not know she had been inserted with one during an abortion procedure at another clinic; Aaliyah attributes this to the IUS clause being buried in the paperwork signed by patients. When I ask them why the IUS is promoted over the IUD, I learn the latter is made of copper and uses the barrier method. Once removed, fertility can resume immediately whereas, with the IUS, the effects of hormonal contraception can result in preventing pregnancy for several months after its removal.
The IUD/IUS – A Technology of Sexual Health
The first vignette is from the perspective of a sales representative, promoting Kyleena to The Centre through the circulation of relevant product information. In this context, the IUS is a form of long-acting reversible contraception (LARC) and commodity, something to be prescribed by physicians in a Toronto sexual health clinic; the fact that the Kyleena is smaller and contains fewer hormones than the Mirena is meant to be a selling point. The contraceptive information and pharmaceutical website can be understood as promoting a choice-based discourse, one which empowers women to select the right contraception which will fit their lifestyle. The second vignette is aboard a mobile clinic, where a poster provokes a hushed conversation between a volunteer, a physician, and a counselor. Dr. Shereen’s contribution draws our attention to how the IUS is presented to physicians (and clients) as the best option for preventing pregnancy, explicitly connecting this to its long-lasting effects, even after removal. Aaliyah gestures towards long-acting reversible contraception’s (LARC) history of racism, sexism, and population control in her client’s story, where the device’s insertion can be understood as coercive. Her story points to the ways in which the IUD/IUS, even as it is promoted as a sexual health and lifestyle choice, is still being used coercively in settings one may not expect.
I draw upon the work of Singer (2016) in framing the IUD/IUS as both a technology of empowerment and a technology of governance. While in the field, I learned there are multiple reasons for having either an IUD or an IUS inserted, pregnancy prevention not always the primary or only concern. The IUS can be used to reduce cramping and reduce the length and degree of bleeding. Either option could be chosen to reduce the number of hormones one is subject to, as the IUD contains zero hormones and the number of hormones released by the IUS is substantially lower than oral contraception. Additionally, the IUD/IUS is also an option for women who do not want their partner to know they are using contraception, as it is less conspicuous than the patch or having to take a daily pill. Within this context, the IUD/IUS as a sexual health technology could be strategically used by women in practice and can be understood as supporting their empowerment through exercising choice.
The beforementioned website promoted by the pharmaceutical representative opens to a sunset-colored page, the hashtag “#mycontraception” and the question “Is your contraception working for you?” This is followed by a series of questions that cover lifestyle, family planning timelines, efficacy, hormones, and menstruation, all of which frame the issue of contraception as an individual choice that should empower the consumer. In some ways, this website parallels the information provided on the poster hanging within the mobile clinic. The IUS and the IUD are presented as the most effective, something both Dr. Shereen and Aaliyah remark on during our conversation. What the poster or website does not mention is how this efficacy is directly tied to notions of user error. Because these devices are inserted and do not require the user to remember to take a daily pill, commit to a schedule of regular Depo-Provera injections, or negotiate condom usage, they are portrayed as the best option even if they offer less autonomy; women cannot stop using an IUD/IUS without the aid of a physician who is trained to remove it, which has caused pause for women in choosing the device (see Gomez, Mann, Torres 2017). Additionally, the story of a young woman having the IUD/IUS inserted without her full informed consent during an abortion procedure, a violent act, reveals how geographical, financial, and social issues involved in accessing abortions resulted in a clinic believing they knew what was best for the young woman.
Understanding and analyzing the IUD/IUS as a sexual health technology reveals its complicated circulation, promotion, and usage. In many ways, this technology is emblematic of the multifaceted nature of sexual health care, simultaneously steeped in discourses of empowerment, choice, and rights while subject to the governance and control of policies, clinics, and pharmaceutical coverage. In understanding the IUD/IUS as a sexual health technology, I point to its multiplicities shaped by both the past and present. Such devices are embedded in histories of population control, capitalism, sexual and reproductive autonomy, state control over female bodies, and patriarchal governance. And yet I wish to emphasize there is also room for its users to exercise agency, hope, and resistance in how they choose (or do not choose) to use it.
References
Davis, Mark
2014 “After the clinic? Researching sexual health technology in context” Culture, Health, and Sexuality. 17(4): 398-411.
Manderson, Lenore (ed.)
2012 Technologies of Sexuality, Identity and Sexual Health. London: Routledge.
Singer, Elyse Ona
2016 “From Reproductive Rights to Responsibilization: Fashioning Liberal Subjects in Mexico City’s New Public Sector Abortion Program” Medical Anthropology Quarterly 31(4): 445-463.
Takeshita, Chikako
2012 The Global Biopolitics of the IUD: How Science Constructs Contraceptive Users and Women’s Bodies. London: MIT Press.
Thiery, Michel
1997 “Pioneers of the intrauterine device” The European Journal of Contraception and Reproductive Health Care 2(1): 15-23.
[1] It should be noted that all the doctors involved in the evolution of the IUD and IUS, devices invented with the goal of preventing pregnancy, were men.
[2] All names used in this piece are pseudonyms to protect participant’s anonymity.

1 Trackback